Brain-Eating Amoeba in Kerala: Symptoms, Locations, Minister’s Advisory
Brain-Eating Amoeba in Kerala: Symptoms, Locations, and Health Advisory from Tamil Nadu Minister M. Subramanian
Reports of brain-eating amoeba infections—medically termed primary amebic meningoencephalitis (PAM)—have sparked concern in parts of Kerala, including Kozhikode and Munnar. Health officials note that the organism can enter the body when people bathe or dive in warm, polluted freshwater and forcefully inhale water through the nose. While rare, the infection can be severe. Tamil Nadu’s Health Minister M. Subramanian has urged the public not to panic, advising people to avoid contaminated water bodies and observe commonsense precautions. He clarified that this is not an infectious disease that spreads from person to person, and that there are no reported cases in Tamil Nadu at present.
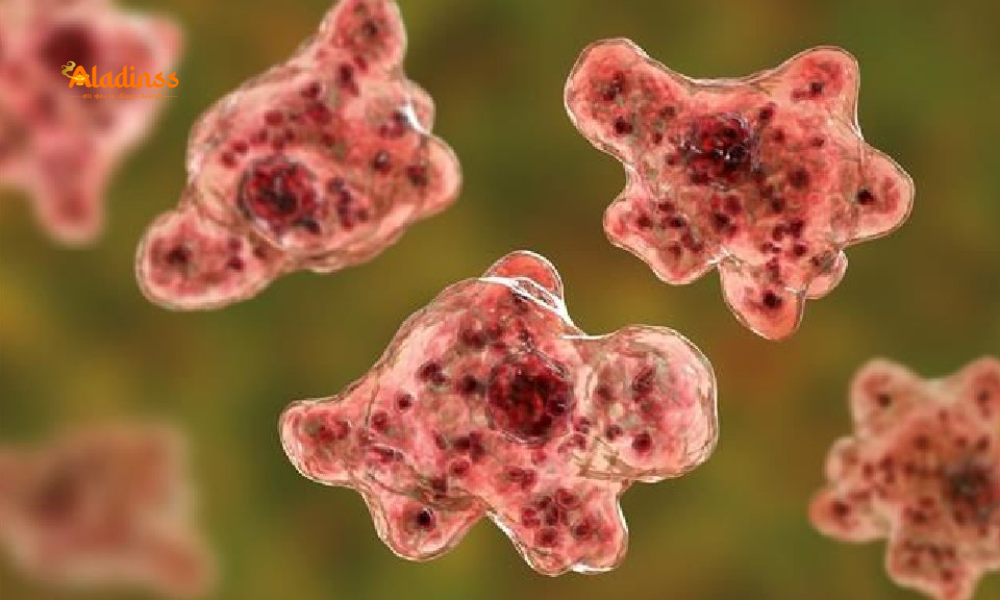
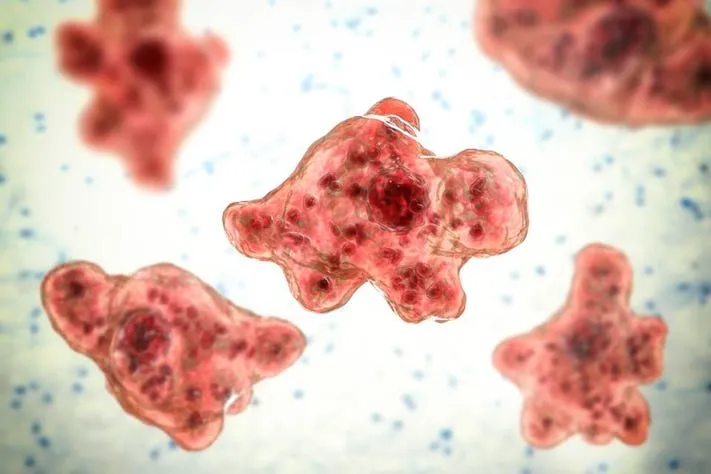
What Is the “Brain-Eating Amoeba” and How Does It Infect Humans?
The so-called brain-eating amoeba is Naegleria fowleri, a free-living microorganism that thrives in warm freshwater such as lakes, ponds, reservoirs, hot springs, under-chlorinated pools, and water accumulated in quarries or man-made pits. The amoeba does not infect via drinking water; instead, it can enter the body when water goes up the nose during activities like diving, jumping, or forceful rinsing. Once in the nasal cavity, the amoeba can travel along the olfactory nerve to the brain, causing primary amebic meningoencephalitis (PAM), a rapidly progressive inflammation of the brain and surrounding tissues.
Where Are Cases Being Reported? Current Focus on Kerala’s Kozhikode and Munnar
Recent reports from Kerala indicate suspected or confirmed instances linked to Kozhikode and Munnar, where locals and visitors often use lakes, ponds, and streams for bathing during warmer months. Experts point out that the risk typically rises in stagnant or slow-moving, warm freshwater, especially when organic matter is high and water treatment is poor. Although the disease remains rare, it receives attention because of its serious clinical course once infection occurs.
Symptoms: What to Watch For and When to Seek Care
Early Signs (Usually Within 1–7 Days After Exposure)
The illness often begins with headache, fever, nausea, and vomiting. People may mistake these symptoms for common viral infections. Some individuals report stuffy nose or discomfort in the nasal passages soon after exposure, especially if they dove or swam underwater and felt water force up the nose.
Progressive Symptoms (Rapid Deterioration)
As inflammation advances, people can develop a stiff neck, sensitivity to light, confusion, loss of attention to surroundings, drowsiness, seizures, and fainting. In severe cases, patients may progress to coma. Medical experts note that deterioration can be very rapid, with serious outcomes reported in many documented cases, sometimes within about 18 days of entry into the body.
Because the disease is rare and can resemble other forms of meningitis or encephalitis, prompt medical evaluation is vital if symptoms occur after recent freshwater exposure, especially with water forced up the nose. Early, specialized treatment may improve outcomes.
“No Need to Panic,” Says Tamil Nadu Health Minister M. Subramanian
Addressing public concerns at the Rajiv Gandhi Government Hospital in Chennai, Health Minister M. Subramanian reiterated that brain-eating amoeba does not spread from person to person. He advised people to be informed, cautious, and calm. Importantly, he stated that there are no reported cases in Tamil Nadu as of now, and emphasized practical preventive measures over fear. His guidance aligns with medical advice to avoid contaminated water bodies and to use safe practices when entering warm freshwater.
Where Is the Amoeba Found? Common Environments and Seasonal Risks
Naegleria fowleri is typically found in warm freshwater and thrives in summer and early autumn when temperatures rise. Risk environments include: — Lakes, ponds, reservoirs, and quarries with stagnant or slow-moving water.
— Streams and waterfalls with warm pools along the banks.
— Poorly maintained or under-chlorinated swimming pools, splash pads, and water parks.
— Untreated groundwater used for recreational purposes.
— Nasal rinsing with unboiled/untreated water (e.g., neti pots) can be risky if water is contaminated.
Why Is Diagnosis Challenging? Rarity and Similarity to Other Illnesses
Clinicians emphasize that PAM is very rare, which paradoxically makes it harder to diagnose promptly. Early symptoms can mirror viral meningitis or bacterial infections, leading to initial treatments that may not target the amoeba. Specialized testing of cerebrospinal fluid (CSF) or advanced molecular diagnostics are often required, and time is critical. Because the disease progresses rapidly, awareness of exposure history—particularly recent freshwater activities—is a valuable clinical clue.
Practical Precautions: How to Lower Your Risk During Freshwater Activities
Smart Choices Before You Enter the Water
Prefer well-maintained, treated pools over untreated freshwater when possible. Avoid bathing in stagnant, warm lakes or ponds, especially after heatwaves. If you do choose natural water bodies, pick spots with visible flow and where local authorities indicate it is safe.
Reduce Nasal Exposure to Water
The key risk is water entering the nose. Keep your head above water where possible. Avoid diving, jumping, or submerging your head in warm, untreated freshwater. Consider using nose clips if you anticipate splashes. For nasal rinsing (e.g., neti pots), use only sterile, boiled and cooled, or properly filtered water.
After Water Exposure
If you experience fever, headache, nausea, vomiting, or unusual neurological symptoms within a week of freshwater exposure, seek prompt medical care and inform clinicians about your recent activities. Early attention to symptoms can aid faster diagnosis and treatment decisions.
Why Health Authorities Urge Awareness, Not Alarm
Despite intense media focus, PAM remains extremely uncommon. Public health experts emphasize risk-aware behavior—avoiding contaminated freshwater, reducing water entry into the nose, and using treated water for nasal hygiene—over fear. The rarity of cases, combined with simple precautions, supports the message from Minister M. Subramanian that there is no cause for panic. Local health departments continue monitoring and advisories to keep communities informed.
Kerala Travel & Community Advisory: Practical Tips for Monsoon and Post-Monsoon Months
For residents and visitors in Kozhikode, Munnar, and nearby districts, choose designated, maintained water sites if you plan to swim. Heed local advisories after heavy rains, when runoff may carry organic material into water bodies. Parents should supervise children who may be tempted to jump into warm, shallow ponds. If a water body looks stagnant, murky, or foul-smelling, avoid entering.
Role of Local Bodies: Water Quality, Signage, and Public Communication
Municipal and panchayat authorities can reduce risk by improving freshwater management, ensuring warning signage where water quality is questionable, and conducting awareness drives ahead of peak heat. Clear guidance—such as “avoid diving,” “use nose clips,” or “do not bathe here”—helps residents make informed decisions. Community groups and tourism operators can support by steering visitors toward safer, monitored swimming locations.
Key Points the Public Should Remember
— The brain-eating amoeba is associated with warm, untreated freshwater, not with drinking water.
— Infection risk stems from water entering the nose—avoid diving or forceful submersion.
— Early symptoms include headache, fever, and vomiting; seek medical care promptly if symptoms follow freshwater exposure.
— The disease is rare; authorities recommend awareness, not panic.
— Tamil Nadu has reported no cases currently; Kerala has issued caution advisories in sensitive spots.
Comment / Reply From
No comments yet. Be the first to comment!