High Cholesterol Symptoms to Watch For

High Cholesterol Symptoms You Shouldn’t Ignore
High cholesterol, often called a "silent killer," can go unnoticed until it causes serious health issues like heart disease or stroke. Once a concern mainly for older adults, it’s now increasingly affecting younger people due to poor diet, lack of exercise, genetics, and lifestyle factors. Recognizing the subtle signs of high cholesterol early can be lifesaving. This article explores key symptoms, their implications, and practical steps to manage cholesterol levels effectively in 2025.
Understanding High Cholesterol

Cholesterol is a waxy substance in the blood, necessary for building cells and producing hormones. However, high levels of low-density lipoprotein (LDL), or "bad cholesterol," can lead to plaque buildup in arteries, increasing the risk of cardiovascular diseases. A 2021 study in the Journal of the American College of Cardiology reported that high cholesterol affects nearly 38% of adults globally, with younger populations increasingly at risk due to diets high in saturated fats and sugars.
The lack of obvious symptoms makes high cholesterol particularly dangerous. Factors such as poor diet, sedentary lifestyles, smoking, and genetic predisposition contribute to elevated levels. Regular cholesterol screenings, especially for those with risk factors like obesity or family history, are critical for early detection and prevention of complications.
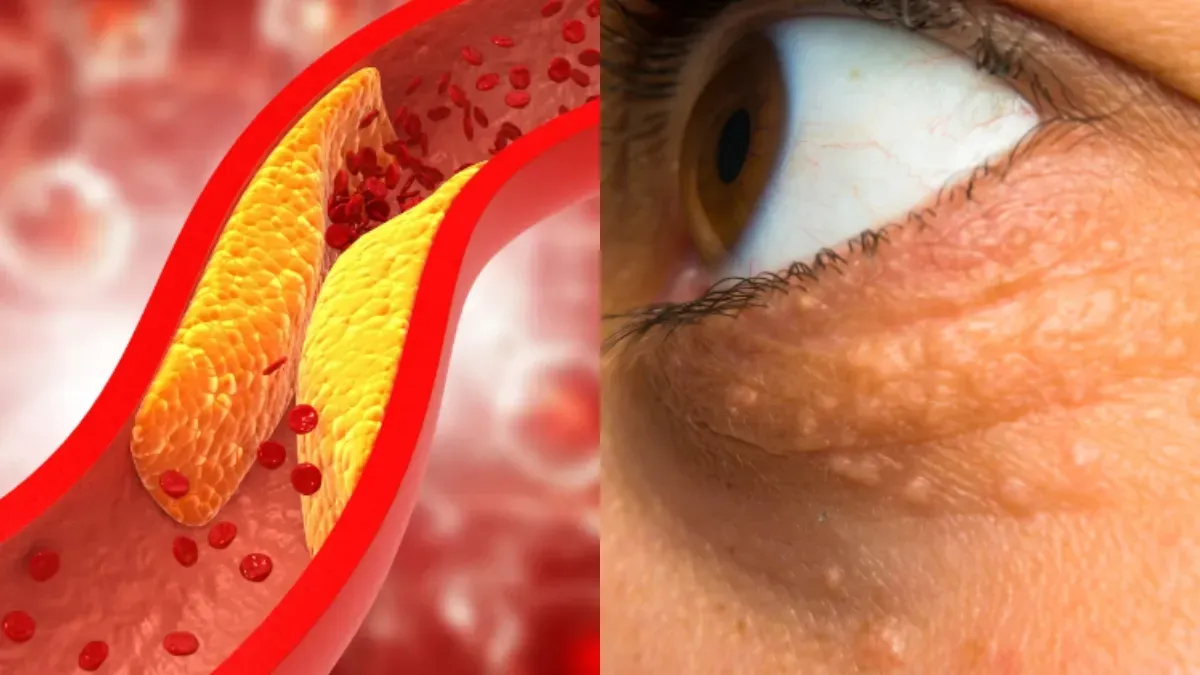
Yellow Patches Around the Eyes (Xanthomas)

One of the most visible signs of high cholesterol is xanthelasma, characterized by soft, yellowish patches or bumps around the eyes. These cholesterol deposits under the skin signal elevated lipid levels and are a warning of potential cardiovascular issues. A 2020 study in the British Journal of Dermatology found that xanthelasma is associated with a 50% higher risk of heart disease, particularly in women and individuals over 30.
While xanthelasma is painless and not harmful, its presence warrants immediate cholesterol testing. These patches are often mistaken for cosmetic issues, but they indicate a need for medical evaluation. Consulting a dermatologist or primary care physician can confirm whether these patches are cholesterol-related and guide further testing, such as a lipid panel, to assess heart health risks.
Chest Pain During Physical Activity

Chest pain or discomfort during physical exertion, known as angina, is a critical symptom of high cholesterol. This occurs when cholesterol plaques narrow arteries, reducing blood flow to the heart. A 2022 study in Circulation reported that angina is an early indicator of coronary artery disease in 20–30% of individuals with high cholesterol, particularly those with additional risk factors like hypertension or smoking.
Younger individuals often misinterpret angina as muscle soreness or fatigue, delaying diagnosis. If chest pain occurs frequently during activities like exercise or climbing stairs, immediate medical attention is essential. Tests such as an electrocardiogram (ECG) or stress test can evaluate heart function, while a cholesterol test can confirm elevated LDL levels. Early intervention can prevent progression to heart attack or stroke.
Also Read: Morning Facial Swelling: Causes & Solutions
Fatty Lumps Under the Skin (Xanthomas)

Fatty lumps under the skin, known as xanthomas, are another visible sign of high cholesterol. These painless lumps, often found on the knees, elbows, hands, or feet, are cholesterol deposits indicating elevated lipid levels. A 2021 study in the Journal of Clinical Lipidology noted that xanthomas are a hallmark of severe hypercholesterolemia, particularly in genetic conditions like familial hypercholesterolemia.
Xanthomas vary in size but are typically soft and may grow over time. Their presence should prompt a lipid panel test to measure cholesterol levels. While harmless, these lumps signal a need for lifestyle changes or medical intervention to reduce cardiovascular risks. A doctor can determine if they are cholesterol-related or due to other causes, ensuring appropriate treatment.
Pain in Legs When Walking

Persistent leg pain during walking, known as claudication, can be a symptom of high cholesterol. This pain results from plaque buildup in the arteries supplying the legs, reducing blood flow and causing discomfort. A 2020 study in the European Journal of Vascular Medicine found that peripheral artery disease (PAD), often linked to high cholesterol, affects 10–15% of individuals with elevated LDL levels.
Claudication feels like cramping or fatigue in the calves, thighs, or buttocks and typically eases with rest. If the pain persists despite rest or lifestyle changes, medical evaluation is necessary. Tests like an ankle-brachial index (ABI) or Doppler ultrasound can assess blood flow and detect arterial blockages. Addressing high cholesterol early can prevent complications like limb ischemia.
Family History of Heart Disease
A family history of heart disease significantly increases the risk of high cholesterol, even in individuals who appear healthy. Genetic conditions like familial hypercholesterolemia can cause elevated cholesterol levels from a young age, leading to premature heart disease. A 2022 study in The Lancet found that individuals with a first-degree relative (parent or sibling) with heart disease have a 40% higher risk of high cholesterol.
If heart disease runs in your family, proactive monitoring is essential. Cholesterol screenings starting in your 20s can detect issues early. Lifestyle changes, such as adopting a heart-healthy diet and regular exercise, can mitigate genetic risks. Consulting a cardiologist for personalized advice, including potential medications, can further reduce the risk of complications.
Managing High Cholesterol
Managing high cholesterol involves a combination of lifestyle changes and, in some cases, medical intervention. Here are key strategies:
Adopt a Heart-Healthy Diet: Reduce saturated and trans fats by avoiding fried foods and processed snacks. Include fiber-rich foods like oats, fruits, and vegetables to lower LDL cholesterol. A 2021 study in Nutrients found that a high-fiber diet reduces LDL by 10–15%.
Exercise Regularly: Aim for 150 minutes of moderate aerobic activity weekly, such as brisk walking or cycling. Exercise boosts high-density lipoprotein (HDL) cholesterol, which helps remove LDL from the bloodstream.
Quit Smoking: Smoking lowers HDL cholesterol and damages arteries. Quitting can increase HDL levels by 10%, according to a 2020 study in the American Heart Journal.
Monitor Cholesterol Levels: Regular lipid panel tests, every 4–6 years for adults or annually for those with risk factors, help track cholesterol levels. Apps like MyFitnessPal can assist in monitoring dietary habits to support cholesterol management.
When to Seek Medical Attention
If you notice symptoms like yellow patches, chest pain, fatty lumps, or leg pain, consult a healthcare provider promptly. Persistent symptoms, especially with a family history of heart disease, require urgent evaluation. Diagnostic tests like lipid panels, ECGs, or imaging can assess cholesterol levels and cardiovascular risk.
For those diagnosed with high cholesterol, medications like statins may be prescribed alongside lifestyle changes. A 2023 study in the Journal of the American Medical Association found that early statin use reduces heart attack risk by 25% in high-risk individuals. Working with a cardiologist or nutritionist can provide tailored strategies to manage cholesterol and prevent long-term complications.
Comment / Reply From
No comments yet. Be the first to comment!